Buprenorphine May Reduce Illicit Drug Use—But Is That Enough?
True success in recovery has always demanded more than simply medicating a person to quell cravings. That’s because the harms of addiction are felt on many levels.

Over the last several years, there has been an extensive push by federal, state, and local agencies to expand access to addiction treatment drugs like buprenorphine. While this measure can save lives in the short term, there are signs that it falls seriously short as a long-term solution to addiction.
One of the primary federal agencies leading this push to provide this medication to those in recovery is the Substance Abuse and Mental Health Services Administration. In December 2022, SAMHSA announced that any practitioner licensed to prescribe opioids by their State can begin treating those addicted to opioids with buprenorphine products.1 Drugs causing opioid use disorder include heroin, fentanyl, oxycodone, hydrocodone, codeine, morphine, or similar drugs.
However, these individuals may be licensed to prescribe painkillers but have no experience treating addicted persons. The vast majority of these practitioners will have no special training in addiction. They may not be able to identify drug-seeking behavior or know how to cope with their patients’ cravings. They have probably never tapered their patients off addictive substances. Nor are they set up to offer counseling, job training, life skills training, etc., because they are simply primary care providers.
The list of these practitioners can include doctors, advanced practice registered nurses, and physician assistants. There is no guarantee that these people will be supported by rehab facilities, counselors, withdrawal specialists, or other support staff. It’s possible that many of these practitioners will simply prescribe a buprenorphine product and leave it at that.
What Is Buprenorphine?
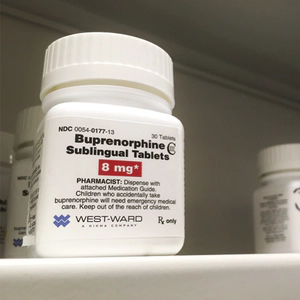
Photo by PureRadiancePhoto/Shutterstock.com
Buprenorphine is an opioid drug. It has been prescribed as a painkiller. It affects the same receptors on the cells that heroin, oxycodone, and morphine do, so that means it has similar painkilling effects. This drug has a very high affinity for these receptors, which means that it will displace morphine, methadone, and other opioids.
While it does create dependence, it is said to create less euphoria for the user. For that reason, it is widely used as a treatment drug for those who wish to stop using drugs like heroin, fentanyl, or oxycodone. Still, it is a drug of abuse, trafficked on the black market, and capable of causing overdose deaths.
In treatment programs, it is used somewhat like methadone. A person gets a dose of buprenorphine every day, and this quells their cravings for the opioids they were using before. There are pills that contain buprenorphine and small pieces of film placed inside the cheek. There is also a once-a-month injection of buprenorphine called Sublocade. In pill or film form, buprenorphine is often mixed with another drug, naloxone, to create a formula called Suboxone.
There are now tens of thousands of practitioners in the U.S. who are licensed to administer this drug. There is no report to tell us how many of these medical personnel simply prescribe this drug and do nothing else to help the individual in front of them fully recover the life they lost to addiction.
Therefore, it must be asked: Is just administering buprenorphine enough?
While asking that question, both the benefits and drawbacks of buprenorphine should be considered.
Benefits
- Being prescribed buprenorphine enables a person to stop searching for, acquiring, and consuming illicit drugs or misusing addictive prescription drugs.
- The person can stop committing crimes to be able to afford their drugs and can begin to normalize their lifestyle.
- They may become more capable of holding a job.
- Buprenorphine quells the insatiable cravings for opioids an addicted person struggles with. As long as they stay on this medication, they will not go into opioid withdrawal.
Drawbacks

- Patients taking buprenorphine can still get high off other drugs, and many do. As noted in one National Public Radio article, one patient taking buprenorphine for her opioid addiction tested positive for cocaine, fentanyl, marijuana, and Xanax.2
- Further, a report from the University of Washington stated: “Stimulant use is common among patients on medications for OUD [Opioid Use Disorder]…People maintained on medications for OUD indicate that they miss the intense effects of short-acting opioids and may have a desire to achieve intoxication and therefore do so with stimulants.”3
- Not every person takes buprenorphine according to doctors’ instructions. According to a study by the National Institute on Drug Abuse, 1.7 million people take buprenorphine products as directed, but 700,000 misuse them.4
- Buprenorphine is involved in a small percentage of fatal drug overdoses. One study attributed 2% of opioid-involved overdose deaths to buprenorphine.5
- It’s not always a successful type of treatment. A five-year follow-up study of those given buprenorphine for opioid addiction found that out of 630 participants, 23 people died by the time of the five-year follow-up. More than 42% were abusing opioids at that point.5
- Even when a person is treated with buprenorphine for as long as 18 months, if their steady treatment is discontinued, they experience a high risk of overdose in the six-month period that follows.6
- The long-term use of buprenorphine comes with its own undesirable side effects, such as headaches, stomach pain, slowed breathing, constipation, insomnia, blurred vision, back pain, decreased sexual desire, tiredness, and confusion.
A Major Failing: Lack of Restoration of Human Qualities and Life Skills
A recovery program with the administration of medications as its primary (and sometimes exclusive) method of treatment fails to offer any service to rebuild life skills or restore the most human of personal qualities of its participants. However, the National Institute on Drug Abuse (NIDA) states:
“Behavioral approaches help engage people in drug abuse treatment, provide incentives for them to remain abstinent, modify their attitudes and behaviors related to drug abuse, and increase their life skills to handle stressful circumstances and environmental cues that may trigger intense craving for drugs and prompt another cycle of compulsive abuse.”[7]

As NIDA notes, it takes much more than medication to recover fully from addiction.
The Urgent Need for Life Skills
According to a report from the World Health Organization, personal change and strong life skills are needed to prevent a relapse into alcohol and drug use.7 The WHO lists the following qualities and skills that must be present to prevent future substance abuse:
Emotional skills:
- Coping with disappointment
- Coping with stress
- Dealing with conflicts
- Dealing with authority
- Dealing with emotions
Thinking skills:
- Creative thinking
- Decision-making
- Critical thinking
- Problem-solving
Social skills:
- Assertiveness
- Awareness of self
- Active listening
- Making and keeping friends and relationships
- Knowing how to cooperate with others
Recovering Human Qualities
There are also certain qualities that must be redeveloped in a person for lasting sobriety. It is possible that these qualities existed before the addiction started. A long time spent addicted to drugs like alcohol, heroin, methamphetamine, high-potency marijuana, and other drugs robs a person of these human qualities:
- Having purpose
- Possessing empathy
- Compassion
- Possessing a strong sense of your own values
- Being worthy of trust
- Being able to trust others
- Sociability
- Honesty
- Self-esteem
- Respect for others and self
- Tolerance
When these qualities are restored or built newly in a person who never developed them, they contribute greatly to a person’s success during addiction recovery.
Recovery From Addiction Must Be Broad-Spectrum
Addiction does not simply create one type of harm. It creates harm on many levels: physical, emotional, financial, familial, and social. It creates barriers to clear thinking and disables one’s ability to cope with the usual stresses of life.
Quelling cravings and preventing withdrawal is not enough improvement for many people. That is only one avenue of many that must be addressed to bring long-term sobriety into being. Medication-assisted treatment by itself is helpful for a transitional phase but does not offer enough therapy for the average person to rebuild strong life skills and recover their most essential human qualities.
What Makes a Drug Rehab Program Successful?

Rehab must help a person overcome cravings and address and rebuild these skills and necessary characteristics. Only a well-rounded drug rehabilitation program can do all that.
A good quality rehabilitation program will specifically address many of the necessary skills and abilities on the lists above. The quality of any rehab program can be determined by the number of people who stay sober after they go home. No program is successful in 100% of the cases. But a higher percentage of success will distinguish a successful program from one that is unsuccessful.
But beware: Many rehab programs only judge their success by how many people get through the set number of days or weeks to complete the program. They don’t monitor how many are still sober one or two years (or longer) later. You have to ask the right questions to get the right answer about the program’s success.
When the percentage of graduates achieving long-term sobriety is high, there is a greater likelihood that the program is providing the broad-spectrum help needed for real recovery. And for most people seeking recovery from addiction, that takes more care, service, support, and help than a prescription for buprenorphine.
Sources:
-
“SAMHSA Proposes Update to Federal Rules to Expand Access to Opioid Use Disorder Treatment and Help Close Gap in Care.” Substance Abuse and Mental Health Services Administration, 2022. SAMHSA ↩︎
-
“A roadblock to life-saving addiction treatment is gone. Now what?” National Public Radio, 2023. NPR ↩︎
-
“Opioids and Stimulants: What Are They and How Are People Using Them?” University of Washington, 2021. U.W. ↩︎
-
“Buprenorphine Misuse Among Adults in the U.S.” National Institute on Drug Abuse, 2021. NIDA ↩︎
-
“Trends and Characteristics of Buprenorphine-Involved Overdose Deaths Prior to and During the COVID-19 Pandemic.” JAMA Network, 2023. JAMA ↩︎ ↩︎
-
“Opioid Overdose Risk Is High After Medical Treatment Ends, Study Finds.” Columbia University, 2019. Columbia University ↩︎
-
“Partners in Life Skills Education.” World Health Organization, 1999. WHO ↩︎







 ®
®