Most Americans are Open to Non-Opioid Pain Relief Post-Surgery
New research shows Americans are becoming more open to utilizing alternatives to opioids when treating pain. Doctors should help their patients avoid addiction risk by making alternative treatments available.

For the first time since opioid pain reliever prescribing began to soar during the late-1990s and early-2000s, a majority of Americans now say they’d be open to trying alternative pain relief options. Such a revelation suggests Americans are becoming more aware of the addiction risks and harmful side effects of opioids. To ensure patients receive safe and effective pain relief, doctors will need to provide patients with alternative treatments.
What the Survey Found
For far too many Americans, addiction begins in the hospital or doctor’s office when patients who suffer from acute or chronic pain are prescribed potent, addictive opioid pain relievers. But with drug overdose deaths reaching an all-time high in 2020 and again in 2021, more Americans than ever before are openly considering alternative pain relief options, even if they feel opioids may still be necessary.
Dr. Luke Elms, a physician at P. Philips Hospital in Orlando, participated in a survey that gauged patients’ openness to alternative pain relief. Quoting Dr. Elms, “When I talk to patients and reassure them that we’re going to be replacing opioids with a much more effective and safe method, and really talk to them about the risks of opioids that have become much more evident with the research that’s come out recently, most patients are very open to the idea.” Dr. Elm’s approach combines acetaminophen, ibuprofen, and muscle relaxers for patients. This approach has the same pain-relieving qualities as opioids like OxyContin and Vicodin but none of the addiction and overdose risk.1
The P. Philips Hospital survey, as a part of that hospital’s Opioid Avoidance Program, found that 68% of patients were open to trying non-opioid pain relief treatments, even as they expressed that sufficiently managing pain was very important to them.
What Percentage of Americans Who Use Prescription Opioids Become Addicted to Them?
The opioid epidemic has wrought untold devastation upon millions of American families, thought by many to be the worst addiction epidemic in U.S. history. Unfortunately, prescribing opioid pain relievers acted as a flashpoint, setting off the escalating crisis and causing thousands of American patients who sought pain relief to become addicted to the drugs that were supposed to help them.
The paper Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use found that at least two million Americans struggle with an addiction involving prescription opioids.2 That figure represents 11% of the 18 million Americans the CDC reports are prescribed opioids. It is a sad state of affairs when America’s most frequently utilized pain relief option has more than a one-in-ten chance of creating a life-ruining addiction.3
When Americans become addicted to their opioid meds, they are at risk for overdose. The National Institute on Drug Abuse reports overdoses involving prescription opioids have been on a steady upwards trend since 1999. At the turn of the century, fewer than 4,000 Americans were losing their lives to opioid pain relievers each year. But in every year since 2010, more than 13,000 Americans have died from painkiller overdoses, with the year 2020 recording 16,416 deaths.4 New research shows Americans are becoming more open to utilizing alternatives to opioids when treating pain. Doctors should help their patients avoid addiction risk by making alternative treatments available.
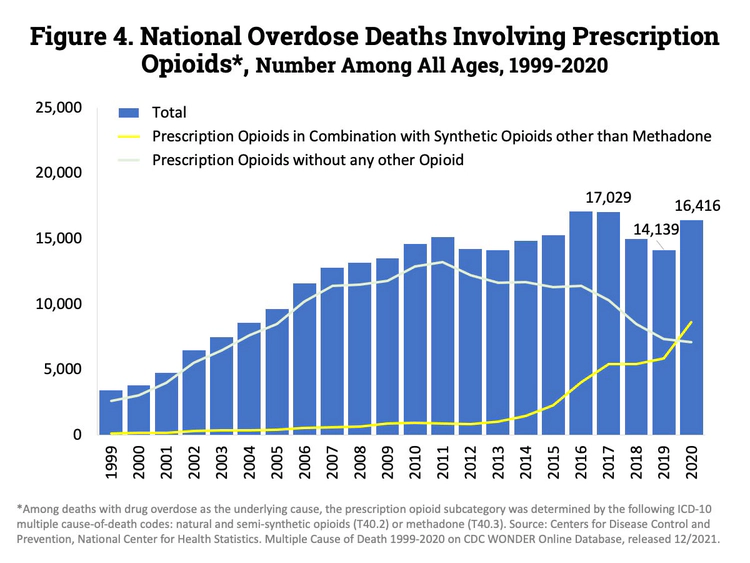
It’s also worth mentioning that prescription opioid addiction set off the broader addiction epidemic and the hundreds of thousands of overdose deaths that followed. The Centers for Disease Control and Prevention found that the opioid epidemic occurred in three waves. The first was a rise in the prescribing of opioid pain relievers between 1999 and 2010, which led to addiction and mass deaths. Once doctors realized what was occurring and began to taper off prescribing between 2010 and 2013, addicts turned to heroin, the second wave. The third wave was marked by the most dramatic spike in deaths as synthetic opioids like fentanyl, tramadol, and other prescribed and illicitly manufactured synthetic opioids entered the drug scene. That stage of the crisis began in 2013 and continues today.5
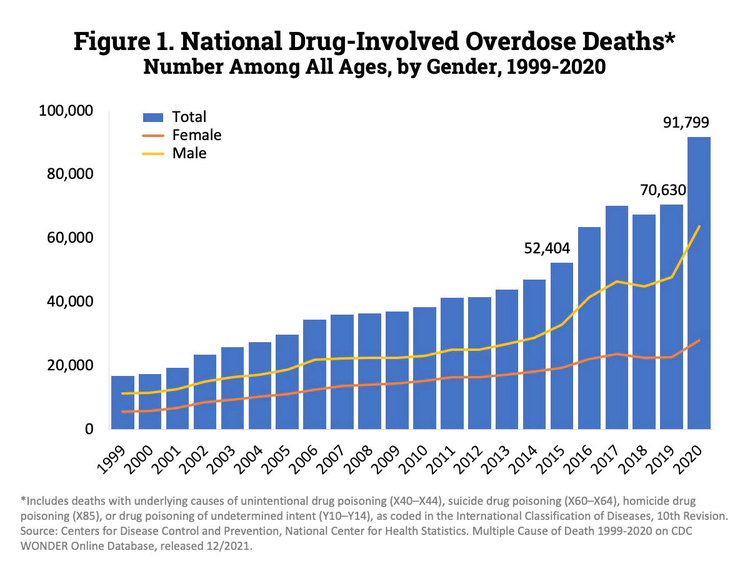
The crippling result of the opioid epidemic has been witnessed in American families suffering year-over-year increases in overdose deaths, with the year 2020 recording a 30% increase in overdose deaths from 2019’s figures (91,799 deaths) and 2021 recording a 15% increase over 2020’s figures (106,000 deaths).
Families Must Demand Alternative Pain Relief Options from Healthcare Providers
As more evidence emerges of the addiction risk and overdose danger attendant with prescription opioids, more Americans are showing interest in effective alternatives for pain relief. In the future, American families must demand medical providers offer treatments that produce sufficient pain relief without the serious health risks and addiction harm attendant with opioids.
Source:
-
OH. “Survey: Patients willing to forgo opioids if their pain can be managed.” Orlando Health P. Philips Hospital, 2022. oh.multimedia-newsroom.com ↩︎
-
NIH. “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use.” National Institutes of Health, 2017. ncbi.nlm.nih.gov ↩︎
-
CDC. “Prevalence of Prescription Pain Medication Use Among Adults: United States, 2015–2018.” Centers for Disease Control and Prevention, 2020. cdc.gov ↩︎
-
NIDA. “Overdose Death Rates.” National Institute on Drug Abuse, 2022. nida.nih.gov ↩︎
-
CDC. “Understanding the Opioid Overdose Epidemic.” Centers for Disease Control and Prevention, 2022. cdc.gov ↩︎







 ®
®