How Did West Virginia Become the State Hardest Hit by the Opioid Epidemic?
West Virginia has become ground zero in a decades-long battle between profits and human lives. In 2020, West Virginia saw 81 deaths for every 100,000 citizens.

The Centers for Disease Control and Prevention published a comprehensive map of the U.S., showing the total drug overdoses in each state and the fatal overdoses per capita. A cursory review of the map confirms what many have feared: while rising drug overdoses have been observed in every state in the nation, the northeast, midwest, southeast, and southwest have been hit the hardest by the addiction epidemic.1
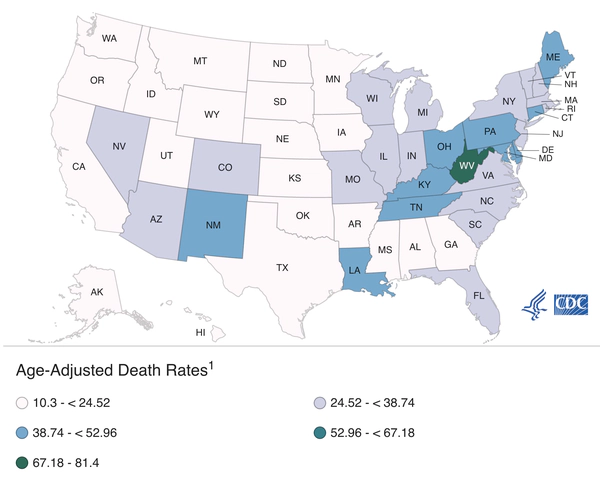
Courtesy of CDC.gov
When looking at the map, viewers are sure to see something else that is quite alarming. West Virginia’s overdose crisis is so overwhelming that West Virginia has a different color code than all the other states. For the numbers, while no other state in the nation exceeds 50 overdose fatalities for every 100,000 people living in that state, West Virginia suffers 81 overdose deaths for every 100,000 residents.
Such an extreme public health crisis, which is far ahead of drug-related struggles in other states, bears examining.
A Summary of the Crisis
The overdose crisis in West Virginia is not new, though the problem is escalating. According to the Drug Enforcement Administration’s special report on West Virginia, the state struggled with 42 overdose deaths for every 100,000 residents in 2015. But by 2020, as the CDC report cited earlier shows, that number almost doubled to 81 deaths for every 100,000 people, significantly higher than the next hardest-hit state, Kentucky, which has 49 deaths for every 100,000. In West Virginia, residents are more than twice as likely to die from a drug overdose than in a car accident.2
Drug fatalities are not the only drug-related harm felt in West Virginia. In January 2020, the Governor’s Council on Substance Abuse Prevention and Treatment published a detailed report on the state’s drug problem. According to that report, the drug crisis is directly linked to statewide increases in liver disease including Neonatal Abstinence Syndrome, hepatitis, HIV, and endocarditis. West Virginia ranks first in the nation for hepatitis B and C, much of which is directly linked to drug use. Twenty-eight of the 220 counties in the U.S. that are considered at high-risk for HIV and/or hepatitis outbreaks are in West Virginia.3
The impact on families has also been severe. According to West Virginia’s public health officials, there is not a family in the state who has not felt the effects of the drug crisis. From a strained foster care system to high rates of babies being born to mothers hooked on drugs, the state is one of the few in the nation facing the real possibility that its next generation will be comprised of young adults exposed to opioid drugs.
Finally, the report also summarizes the economic toll of the drug problem. Drug addiction costs West Virginians approximately $8.8 billion yearly, at least one-eighth of the state’s total economy. That cost comes from state spending on health care, substance use treatment, and criminal justice, plus the societal burden of fatal overdoses and lost worker productivity.
The report’s findings perfectly summarize how all West Virginians are affected by the drug crisis. Quoting the authors, “The economic impact of productivity loss for non-fatal substance use disorders has a reported cost of $316 million dollars and 1,206 jobs to the state, while the economic impact of productivity loss due to overdose fatalities carries an additional cost of $322 million and 5,905 jobs. The impact is also seen in a 12% economic drag on the state’s Gross Domestic Product (GDP), more than double that of the next highest state of Maryland where substance use disorder-related costs consumed 5.4% of its GDP.” These costs equate to a per-capita price tag of $4,793 per resident per year, higher than anywhere else in the nation.
Reasons Why West Virginia is the State Hardest Hit by the Opioid Epidemic
Drug addiction is a personal crisis, and there should be no stereotyping or stigmatizing that drug abuse only affects certain types of people in specific circumstances. However, it has been observed that several individuals in the same geographic area may struggle with similar life factors that could lead to drug abuse, even if each person’s life story and personal struggle is unique to them.

West Virginia (and much of Appalachia) is a good example of this. While drug addiction can affect anyone on any rung of the income ladder, economic struggles and joblessness often create painful life circumstances that cause people to turn to drug abuse as a coping mechanism. In West Virginia, a state with the 15th highest unemployment rate and the fourth highest poverty rate, poor economic conditions may create the conditions for drug abuse. Then drug abuse further exacerbates harsh economic conditions, thus creating a vicious cycle of poverty.4
Another factor is that West Virginia has long been a working-class state, with many of its adults employed in jobs that involve manual labor like coal mining, timbering, and manufacturing, leading to high rates of chronic physical pain among the state’s working-age adults.
A scandal erupted during the 2000s and 2010s in which pharma companies flooded West Virginia with opioid pain relievers, compelling local doctors to prescribe highly addictive painkillers for West Virginia’s working-class adults, creating a micro epidemic of addiction, self-medication, replacement of painkillers with cheaper opioids like heroin and fentanyl, and resulting overdoses.5
Yet another factor to consider is West Virginians’ relative lack of access to health care services. That leads to residents self-medicating, not seeking help when they should, not having access to addiction treatment services, and not being able to seek help when an overdose occurs. West Virginia is a ‘medical desert’ with a 19% poverty rate, 9% of the population living with zero health coverage, 19% of adults not having a primary care provider, 14% of residents being unable to afford medical care, and 21% not receiving routine health checkups.6
The Importance of Working Together in West Virginia
The drug problem has become so deeply entwined in all aspects of life in West Virginia that there is no quick fix or single solution to relieve the state’s addiction epidemic. As reports suggest, every family in the state knows someone harmed by the drug problem. Now more than ever, those families must come together and ensure their addicted loved ones receive professional help.
Addiction is a nightmare, but it does not have to be permanent. West Virginia faces numerous challenges in overcoming its addiction emergency, but the best solution is to ensure those who are addicted receive help at residential drug treatment centers. Family members of addicts should work closely with other families, loved ones, friends, and public health officials to ensure addicted individuals get help before it is too late.
Sources:
-
CDC. “Drug Overdose Mortality by State.” Centers for Disease Control and Prevention, 2020. cdc.gov ↩︎
-
DEA. “The West Virginia Drug Situation.” Drug Enforcement Administration, 2017. dea.gov ↩︎
-
DHHR. “West Virginia 2020-2022 Substance Abuse Response Plan.” Department of Health and Human Resources, 2020. dhhr.wv.gov ↩︎
-
BLS. “Unemployment Rates for States.” Bureau of Labor Statistics, 2022. bls.gov ↩︎
-
DHHR. “Statistics about the population of West Virginia.” Department of Health and Human Resources, 2018. dhhr.wv.gov ↩︎
-
WP. “Judge rejects claim distributors fueled W.V. community’s opioid crisis.” Washington Post, 2022. washingtonpost.com ↩︎







 ®
®